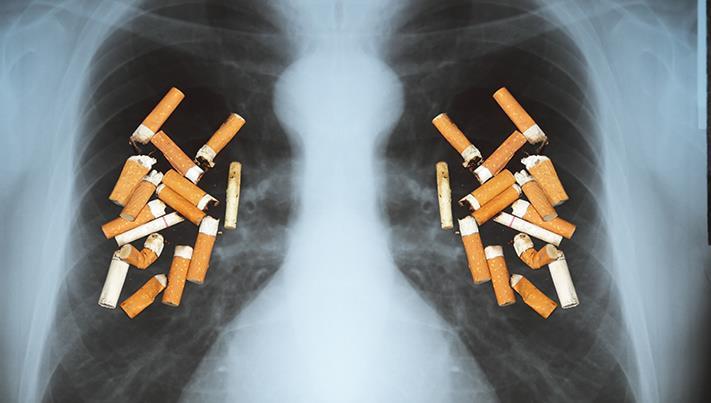
Three out of four patients diagnosed ‘too late’
Variations in lung cancer care ‘cannot be tolerated’ and many people face ‘unwarranted’ delays in treatment, says a new report published today (22 November 2018) by the UK Lung Cancer Coalition (UKLCC).1
According to the report, just a quarter (27%) of lung cancer patients in England receive an early diagnosis (stage I or II) ‘ and only around three quarters of lung cancer patients (72.6%) get treated within the current 62-day national cancer waiting time standard.1
‘Three out of four people with lung cancer are diagnosed too late to be suitable for potentially curative treatment’ says Professor Mick Peake (Chair), Clinical Director, Centre for Cancer Outcomes, Cancer Collaborative, UCLH and Chair of the UKLCC’s Clinical Advisory Group. ‘Unwarranted delays in treatment, even at the early stages, can allow a tumour to grow by just a few millimetres which can have a dramatic effect on someone’s chance of survival.’
Lung cancer is the biggest cancer killer in the UK for both men and women ‘ with five-year survival rates consistently lagging behind many other countries in Europe. England currently ranks 26th out of 29 countries.3
Titled ‘Millimetres Matter’, the UKLCC report is calling for local cancer services to implement the National Optimal Lung Cancer Pathway (NOLCP), an NHS England initiative which advocates a standardised care pathway for lung cancer patients, wherever they live, as well as faster access to diagnostic tests and treatment and reduced waiting times.4
The UKLCC believes putting the NOLCP into action, will help achieve its ambition of boosting five-year UK lung cancer survival to 25% by 2025.*
Patients diagnosed at the earliest stage of lung cancer are almost five times more likely to survive a year from diagnosis than those diagnosed in the later stages. 1
Currently, lung cancer patients in the UK are diagnosed with more advanced disease than many other countries and a third first reach specialist care following an emergency admission to hospital.5
Studies show there is a 16% increase in mortality if the time from lung cancer diagnosis to having surgery is more than 40 days – putting lives unnecessarily at risk.1
‘A delayed diagnosis means patients having their worst fears dragged out, with thousands of people being left in an appalling state of limbo,’ adds Richard Steyn, Consultant Thoracic Surgeon; Deputy Medical Director, University Hospitals Birmingham NHS Foundation Trust; Honorary Associate Professor, University of Warwick and Chair of the UKLCC. ‘Despite improvements, we are still failing patients in England and the rest of the UK. More must be done to address the poor lung cancer survival in this country. Therefore, it is imperative that all hospital trusts adopt the National Optimum Lung Cancer Pathway.’
In addition to urging adherence to the National Optimal Lung Cancer Pathway, the UKLCC’s report sets out a series of practical, real-life examples and case studies of how NHS trusts are already implementing elements of the NOLCP. These include a centralised booking system for diagnostic tests; appointment of a treatment pathway coordinator; inter-trust lung cancer referrals and providing patient travel for long-distance hospital appointments.1
To access the report, visit: www.uklcc.org.uk?