Innovation & Medtech
Browse Posts in Various Categories

Real World Evidence and Responsible AI Practices…
Artificial intelligence (AI) has the potential to transform healthcare delivery through its impact on healthcare systems, treatment outcomes, and patient…
View Article
Automation Will Play a Critical Role in…
The healthcare industry is inundated with challenges, from an ageing population and higher cost of care to poor processes between…
View Article
Hundreds of Sickle Cell Patients to Benefit…
Children, young people, and adults across England suffering from sickle cell disease will soon benefit from better care closer to…
View Article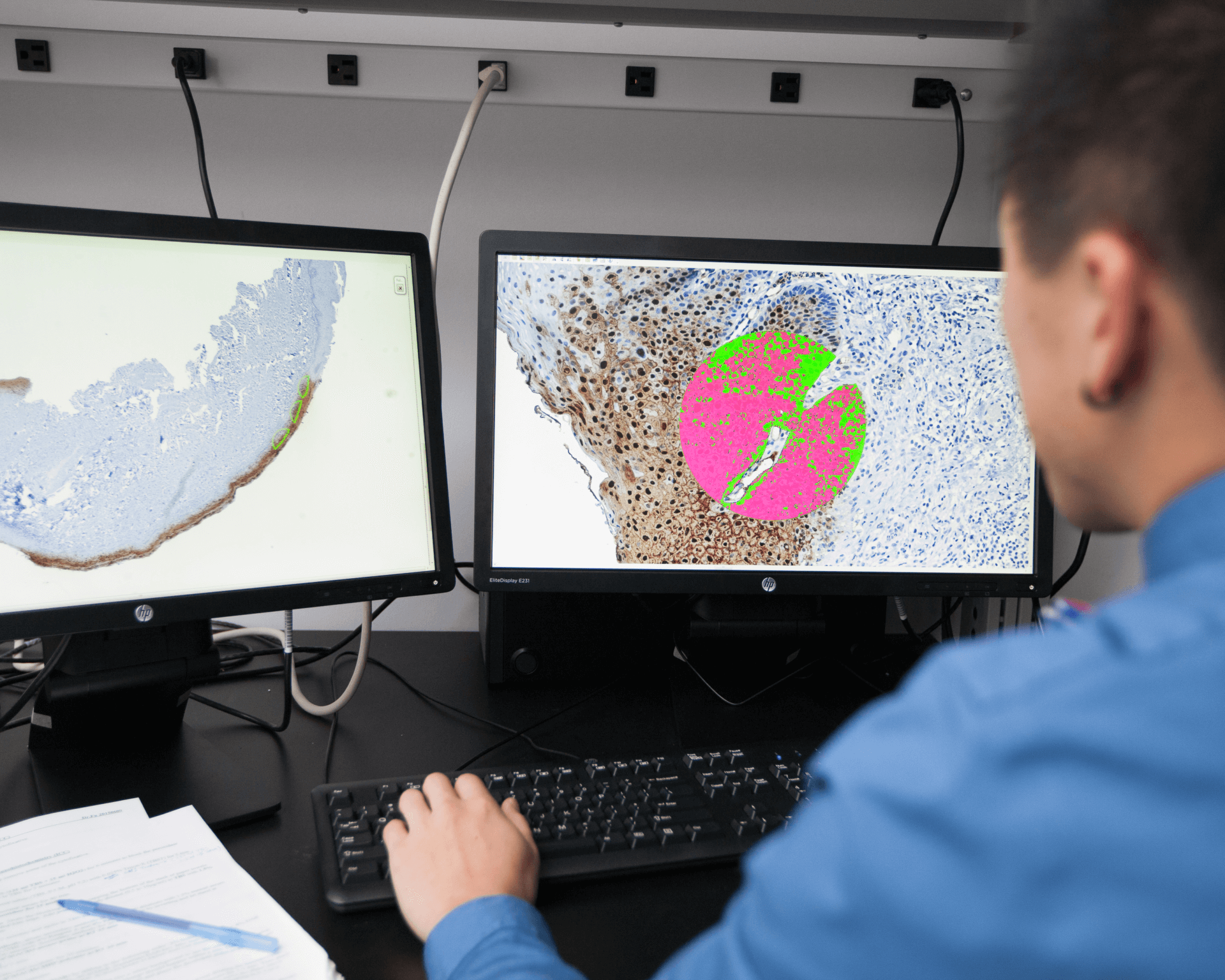
Accurately Predicting Your Risk of Developing Oral…
Proteocyte AI is a Canadian medtech company that uses proteomics to individually assess cancer risk in vulnerable patients. The STRATICYTE…
View Article
Uncovering the Hidden ROI of Pharmacovigilance Literature…
In pharmacovigilance, the perception that investment in medical literature monitoring yields a low return on investment (ROI) is not uncommon.…
View Article
Blockchain Technology Can be Used to Prevent,…
Healthcare is one industry where records are of utmost importance as they help in preventing and reducing medical error.
View Article
Multi-Jet Fusion Technology: A Medical Marvel?
3D printing, or additive manufacturing, is transforming the medical world, with multi-jet fusion technology being heralded as a disruptive game-changer.…
View ArticleExplore Other Categories